By Renee Cowan, MD, MPH
GYN Oncologist, Woman’s Hospital
You’ve probably heard a lot in mainstream news and on social media about breast cancer. Chances are, you know someone who has experienced it and/or have been educated on the importance of mammograms. While breast cancer is a major health concern for women and is the leading new cancer diagnosis in women, did you know there are other cancers that women are at risk for developing?
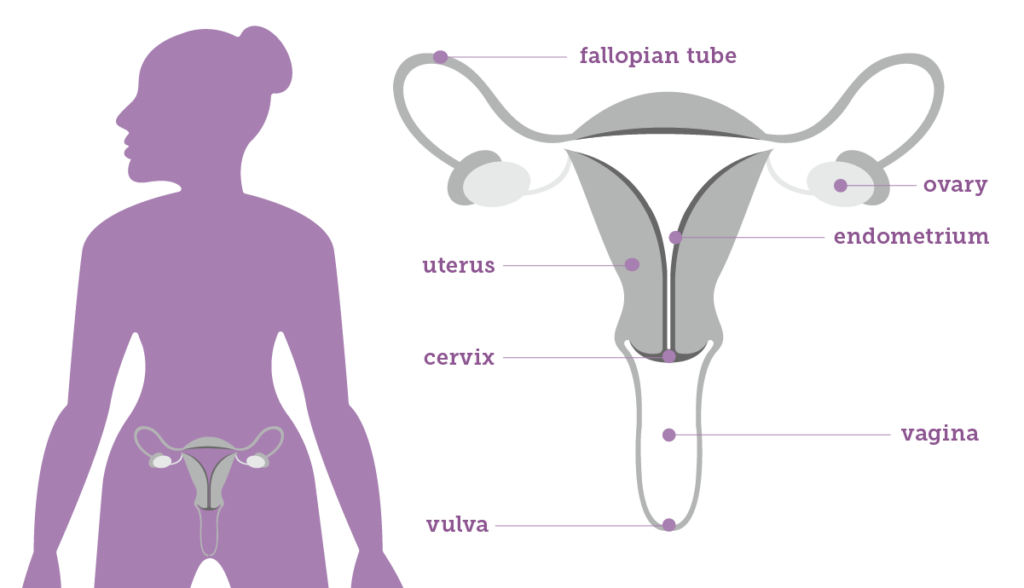
Over 100,000 women are diagnosed with gynecologic, or GYN, cancer in the United States each year. GYN cancer includes any cancer that starts in a woman’s reproductive organs which includes the cervix, uterus, fallopian tubes, ovaries, vagina, and vulva. Uterine cancers are the 4th most common cancer diagnosis in women each year while ovarian cancers are the 5th leading cause of cancer deaths in women. While there is no sure way to prevent these types of cancers, there are some steps you can take to lower your risk and increase your awareness.
Live a Healthy Lifestyle
The best thing a woman can do to protect herself from a GYN cancer or any cancer is to live an overall healthy lifestyle. All the things we’re constantly told to do — eat lots of vegetables, get enough sleep, decrease stress, avoid smoking, minimize alcohol intake, exercise regularly, maintain a healthy body weight– those are the things that increase your health and decrease your chance of cancer in general. However, this is especially important when it comes to GYN cancer because obesity causes increased estrogen production and chronic inflammation which increases the risk of the most common GYN cancer, endometrial cancer (a cancer of the lining of the uterus).
Know Your Normal
When it comes to female health, it can be hard to know what’s normal and what’s not. No one knows your body better than you, so it is important to pay attention and know your normal so you can recognize when and if something is off. Each cancer type has different symptoms and some of them can be very vague or non-specific, but bloating, pain/pressure, feeling too full too fast, and unusual bleeding are some common warning signs you should monitor. Since there is no simple and reliable way to screen for most gynecologic cancers except cervical cancer, it is especially important to know the warning signs and talk to your doctor if something doesn’t seem right. Here are some red flags that warrant calling your doctor right away: vaginal bleeding after menopause, bleeding after sexual intercourse, foul smelling vaginal discharge, a growing pelvic mass or fibroids getting significantly bigger after menopause.
Know Your Family History
You may have heard that cancers can run in families and that is true. Multiple GYN cancers can be related to your DNA or your genes. Try to get to know your family history and what cancers your family members may have been affected by. Depending on your family history, especially if there are multiple members of your family who suffered from breast and ovary or colon and uterine cancers, you may be eligible for genetic testing. Genetic testing may seem daunting, but oftentimes uncovering genetic abnormalities can help your physician recommend a treatment or surveillance program that could prevent a cancer from developing or catch it while it is in its earliest stages.
Routine Screening Tests and Gynecologic Exams
- Pap Test: Cervical cancer is the only GYN cancer with a reliable screening test. The Pap test or smear is a procedure used to collect cells from the cervix so that they can be looked at closely in the lab to find cancerous and precancerous cells. If precancerous lesions are identified, they can be removed before they progress to cancer. Pap test guidelines change frequently as we learn more about the disease process, but usually start around 21 years of age and are conducted every 3-5 years. Be sure to consult with your gynecologist and see them every year.
- HPV Test: The HPV test, often performed at the same time as the Pap Test, looks for infection by high-risk types of HPV that are more likely to cause pre-cancers and cancers of the cervix. Similarly, the guidelines do evolve so be sure to consult with your gynecologist. Additionally, there are multiple HPV vaccines available that offer protection from many of the strains of HPV responsible for causing cancer.
- Pelvic Exams: We cannot mention this enough–Visit your gynecologist regularly for a checkup! Though pelvic exams can be uncomfortable, a thorough annual exam can detect precancerous lesions of the vulva, vagina, or cervix or a mass in your pelvis that is new and/or growing and shouldn’t be present. A detailed history (or discussion with your physician) can reveal abnormal or post-menopausal bleeding that your physician can address immediately.
To learn more about GYN cancer or our Woman’s GYN Oncology team visit our website. And most importantly, if you or any woman you know is concerned about GYN cancer or a symptom, talk to your primary care physician or gynecologist right away or make an appointment with one of ours!